Blog

Written by Julie Bick, Ph.D.
When it comes to treating chronic conditions, the effectiveness of prescribed medications is central to symptom management. However, the reality is that not all medications work equally well for everyone. Ineffective medications can not only fail to treat the condition but can also exacerbate it, leading to a host of additional health complications.
Ineffective medications can result from range factors, and in this blog, we review some of the studies highlighting the personal impact of ineffective medications on patients, as well as the economic burdens this has for us all.
Understanding the Problem
When it comes to medications, there really is no universal approach. But most of us have no idea just how many individuals don’t respond to drugs in the intended way.
Fig. 1. highlights the extent of this issue across several classes of medicines. This clearly demonstrates that as the concept of precision medicine is now becoming more mainstream within healthcare, the idea of one-size-fits all therapies is a thing of the past.
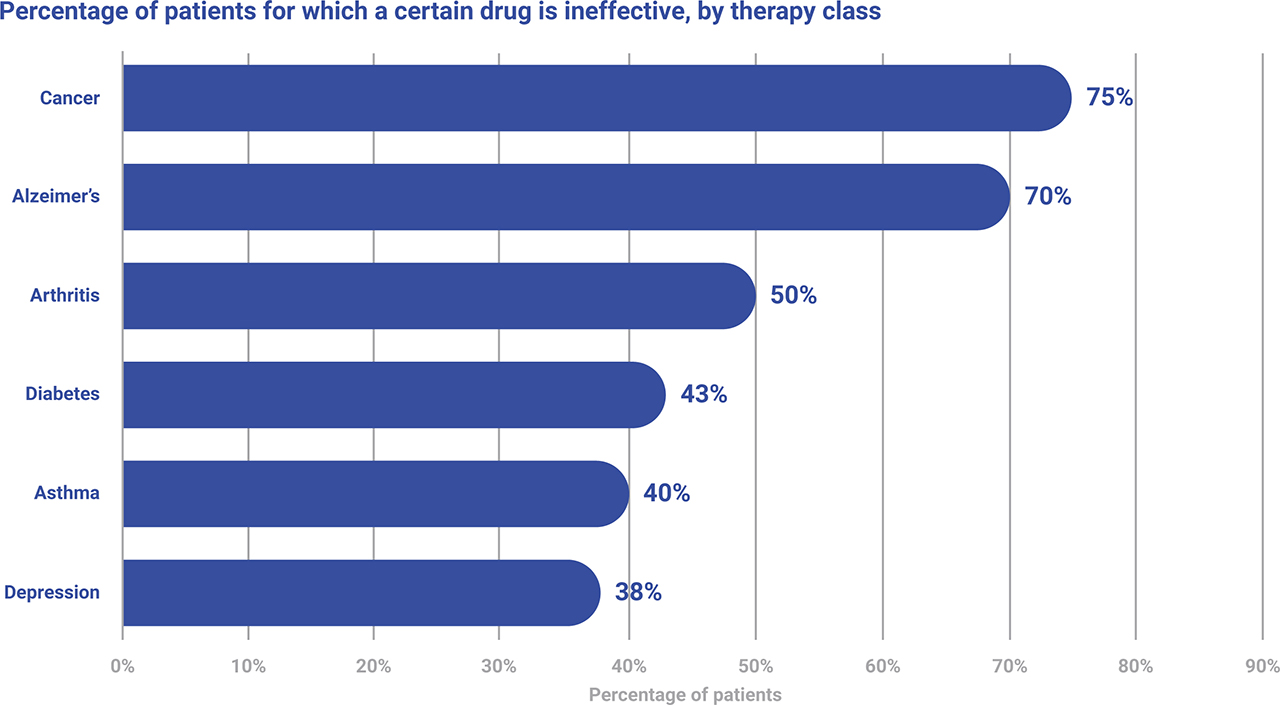
Fig. 1. The Percentage of the patient population for which a particular drug in a class is ineffective.
The Human Aspect
The term ‘Ineffective medications’ refers to drugs that do not produce the intended therapeutic effect in a patient. The reasons behind this vary, and each require different approaches to address and improve, but human behavior is a big part of the problem.
As with everything in life, communication is key- and sadly, ineffective physician to patient communication can be dangerous or even deadly. In an ideal world, the physician would have time to thoroughly discuss a patient’s symptoms, health history, medications, health habits and lifestyle (diet, exercise, nutritional supplements) in order to provide optimal care. The reality is very different, and primary care physicians spend only an average of 18 minutes with their patients, and patients are suffering because of it (Ha and Longneck, 2010) either by receiving an incorrect or incomplete diagnosis or inappropriate drug selection (Neprash et. al. 2023).
The issue isn’t only with the physicians though, the Centers for Disease Control (CDC) reports that a staggering 80% of patients do not take their medications as prescribed, and an estimated 125,000 people die annually from issues related to inappropriate medication use. The high cost of medications is only compounding this problem, with an estimated 8.2% of adults between the ages of 18-64 who are prescribed medications, not taking them as prescribed due to the cost, either by skipping doses, taking less medication than prescribed or delaying filling a prescription (Mykyta and Cohen, 2021). This nonadherence is increasing the risk of disease advancement to more serious conditions, that ultimately require additional treatment. To highlight this, a 2019 Gallup survey found that 58 % of Americans have negative view with little or no confidence in the pharmaceutical industry, a sentiment that has only been exacerbated by experiences with ineffective treatments (https://news.gallup.com/poll/266060/big-pharma-sinks-bottom-industry-rankings.aspx).
What is emerging now is a third and highly significant aspect to medication efficacy, that lies within our genes. The field of pharmacogenomics (PGx) examines a patient’s genetic profile encoding the mechanisms for drug absorption, metabolism and excretion, and is being used to help prescribing physicians identify the right drug, at the right dose for the individual. It is not a new area of medicine, but it is one now gaining traction with all stakeholders within the healthcare industry who see PGx as a cost-effective means of wide-spread genetic testing to support safe and effective medication protocols, that ultimately will lead to safer therapeutic interventions as well as help manage medication costs. Incite Health is offering a comprehensive PGx test that covers more than 70% of commonly prescribed medications in the US. This test provides a lifetime of medication management guidance to support optimal health through personalized therapeutic intervention.
PGx-Driven Real World Solutions
Two of the most prevalent applications of PGx-driven medication guidance are with commonly prescribed anticoagulants and antidepressants.
PGx guided medication management for anticoagulants like warfarin and clopidogrel, involves several key genes that affect drug metabolism and response. CYP2D9 encodes an enzyme that metabolizes warfarin, and variants of this gene can affect the rate at which warfarin is broken down. This is particularly important since warfarin has a narrow therapeutic index, meaning that the effective dose is close to the toxic dose. Another key gene for warfarin safety and efficacy is VKORC1, which encodes the vitamin K epoxide reductase complex subunit 1, the target for warfarin. Variants in VKORC1 can influence warfarin sensitivity, and impact the dose required to achieve therapeutic anticoagulation. PGx profiling in combination with clinical the INR blood test (International Normalization Ratio) are helping physicians more effectively manage warfarin dosing for their patients.
Similarly, PGx can be used to guide dosing for clopidogrel, and more importantly identify patients for whom clopidogrel should not be given due to a risk of serious drug-gene interactions. The gene CYP2C19 encodes the enzyme primarily involved in clopidogrel metabolism and variants in CYP2C19 can influence the effectiveness of the drug due to its’ poor metabolism. In addition, ABCB1 encodes a P-glycoprotein which influences the adoption and distribution of range of drugs, including clopidogrel.
It is now well described that the efficacy of antidepressants can vary widely among individuals. Clinical research has shown that genetic factors can explain up to 42% of the variability in antidepressant response. PGx testing for variations in the CYP2D6 and CYP2C19 genes is being used to guide the selection of the most effective antidepressant for each patient; these include the optimal selection of serotonin re-update inhibitors (SSRIs) and tricyclic antidepressants (TCAs). In addition, PGx profiling of other gene variants including CYP1A2, SLC6A4, COMT and HTR2A is helping physicians to select specific drug doses to minimize detrimental side effects more effectively. All of this is working to support greater drug safety and efficacy and help reduce the frequency and impact of prescribing ineffective mental health medications to patients.
The Impact of Fake or Substandard Medications.
One of the most direct impacts of ineffective medications globally is on morbidity and mortality rates. A study by the World Health Organization (WHO) estimates that around 10% of medications globally are substandard or falsified, contributing significantly to morbidity and mortality rates, especially in low and middle-income countries. (Read the full report here: https://iris.who.int/bitstream/handle/10665/326708/9789241513425-eng.pdf). This is a complex issue, driven by intellectual property rights, poor pharmaceutical governance and a global supply chain with little to no oversight. Sadly, despite efforts there is no easy solution, since the global coordination, standardization and surveillance of medication quality is an incredibly high bar to achieve (Ozawa et. al. 2018).
Ineffective Medications are Exacerbating Chronic Conditions, Eroding Patient Health and Increasing Healthcare Costs.
It is well documented that ineffective medications can worsen chronic conditions. For example, patients with hypertension or diabetes relying on ineffective drugs may experience uncontrolled blood pressure or glucose levels, leading to complications such as heart disease, kidney failure, or strokes. A review published in Patient Prefer Adherence (Hamrahian et. al. 2022) highlighted the impact of hypertension worldwide, and the heavy burden of ineffective medication management. They reviewed the results from many clinical studies demonstrating the prevalence and risks of ineffective antihypertensive medications that results in patients not achieving blood pressure control and putting them at higher risk of developing other chronic conditions and comorbidities (Holt et. al. 2010; Miller 1997).
Furthermore, the chronic use of ineffective medications can lead to increased anxiety and depression among patients. For instance, patients with chronic pain who do not find relief from prescribed medications may experience worsening mental health conditions, and there are many clinical studies demonstrating that patients with ineffective pain management are more likely to report symptoms of depression and anxiety, requiring additional medications to manage their mental health (Fishbain et. al. 1997).
The economic impact of ineffective medications is profound, affecting both individuals and healthcare systems. Direct costs include the expenses incurred from purchasing ineffective medications, additional medical consultations, diagnostic tests, and hospitalizations. According to a report by the Institute of Medicine, medication errors, including the use of ineffective drugs, cost the U.S. healthcare system approximately $17 billion annually (Van Den Bos et. al. 2011). There are also indirect costs that stem from lost productivity due to illness, prolonged treatment periods, and premature deaths. The economic burden of antibiotic resistance alone is estimated to be around $55 billion per year in the U.S., with $20 billion attributed to direct healthcare costs and $35 billion to lost productivity (Prestinaci et. al. 2015).
The Role of Regulatory Bodies
Regulatory bodies play a crucial role in ensuring the efficacy and safety of medications. The U.S. Food and Drug Administration (FDA), the European Medicines Agency (EMA), and other regulatory agencies worldwide implement rigorous evaluation processes for drug approval. However, challenges remain. The prevalence of substandard and falsified medications poses a significant challenge. The WHO reports that one in ten medical products in low and middle-income countries is substandard or counterfeit, leading to ineffective treatment and adverse health outcomes. Efforts to combat this issue include the implementation of stricter regulations, improved surveillance, and international cooperation.
Implementing systems for continuous monitoring and feedback can help identify and address issues with medication effectiveness early. Electronic health records (EHRs) and real-world evidence (RWE) are invaluable tools in this regard. They enable healthcare providers to track patient outcomes, adjust treatments as needed, and identify patterns of ineffective medication use across a broader population. The incorporation of genetics such has PGx variant profiles within this data, will ultimately help patients.
Final Thoughts
The future of medication effectiveness lies in innovation, collaboration, and patient-centric approaches. Advancements in biotechnology and artificial intelligence (AI) are revolutionizing drug development. Despite potential risks, it is well accepted that AI-driven drug discovery can expedite the identification of potential drug candidates, predict their efficacy, and personalize patient’s treatment. For example, machine learning algorithms can analyze vast datasets to identify biomarkers that predict patient responses to specific drugs, enhancing the effectiveness of new medications (Babel et. al. 2021). Even The White House is placing AI at the forefront of healthcare innovation (https://www.whitehouse.gov/briefing-room/blog/2023/12/14/delivering-on-the-promise-of-ai-to-improve-health-outcomes/) with an executive order providing guidelines for AI’s safe and responsible implementation in the healthcare sector and others (https://www.whitehouse.gov/briefing-room/presidential-actions/2023/10/30/executive-order-on-the-safe-secure-and-trustworthy-development-and-use-of-artificial-intelligence/)
Global health initiatives are crucial in addressing the challenges posed by ineffective medications, especially in low and middle-income countries. International organizations such as WHO, along with governments and non-governmental organizations, are working towards improving drug quality, enhancing regulatory frameworks, and increasing access to effective medications. Raising awareness and educating both healthcare providers and patients about the importance of medication effectiveness is vital. Healthcare professionals need to stay informed about the latest developments in pharmacogenetics, personalized medicine, and drug resistance. Patients, on the other hand, should be empowered to actively participate in their treatment, adhere to prescribed regimens, and communicate openly with their healthcare providers.
The impact of ineffective medications on patients is profound, spanning health outcomes, economic burdens, and psychological effects. Understanding the factors contributing to medication ineffectiveness and implementing strategies to address them is crucial in improving patient care and outcomes. As the field of precision medicine continues to evolve, the integration of personalized approaches, advancements in drug development, and global health initiatives hold promise in mitigating the challenges posed by ineffective medications. Through collaborative efforts and continuous innovation, we can plan for a future where every patient receives the most effective, safest and tailored treatment possible.
References
- Ha JF, Longnecker N. Doctor-patient communication: a review. Ochsner J. 2010;10(1):38-43
- Neprash HT, Mulcahy JF, Cross DA, Gaugler JE, Golberstein E, Ganguli I. Association of Primary Care Visit Length With Potentially Inappropriate Prescribing. JAMA Health Forum. 2023;4(3):e230052. doi:10.1001/jamahealthforum.2023.0052
- Mykyta L, Cohen RA. Characteristics of adults aged 18–64 who did not take medication as prescribed to reduce costs: United States, 2021. NCHS Data Brief, no 470. Hyattsville, MD: National Center for Health Statistics. 2023. DOI: https://dx.doi.org/10.15620/cdc:127680
- Ozawa S, Evans DR, Bessias S, Haynie DG, Yemeke TT, Laing SK, Herrington JE. Prevalence and Estimated Economic Burden of Substandard and Falsified Medicines in Low- and Middle-Income Countries: A Systematic Review and Meta-analysis. JAMA Netw Open. 2018 Aug 3;1(4):e181662. doi: 10.1001/jamanetworkopen.2018.1662. PMID: 30646106; PMCID: PMC6324280.
- Hamrahian SM, Maarouf OH, Fülöp T. A Critical Review of Medication Adherence in Hypertension: Barriers and Facilitators Clinicians Should Consider. Patient Prefer Adherence. 2022 Oct 7;16:2749-2757. doi: 10.2147/PPA.S368784. PMID: 36237983; PMCID: PMC9552797.
- Holt EW, Muntner P, Joyce CJ, Webber L, Krousel-Wood MA. Health-related quality of life and antihypertensive medication adherence among older adults. Age Ageing. 2010;39(4):481–487. doi: 10.1093/ageing/afq040
- Miller NH. Compliance with treatment regimens in chronic asymptomatic diseases. Am J Med. 1997;102(2):43–49. doi: 10.1016/S0002-9343(97)00467-1
- Van Den Bos J, Rustagi K, Gray T, et al. The $17.1 Billion Problem: The Annual Cost Of Measurable Medical Errors. Health Aff. 2011;30(4):596-603. doi:10.1377/hlthaff.2011.0084.
- Prestinaci F, Pezzotti P, Pantosti A. Antimicrobial resistance: a global multifaceted phenomenon. Pathog Glob Health. 2015;109(7):309-18. doi: 10.1179/2047773215Y.0000000030. Epub 2015 Sep 7. PMID: 26343252; PMCID: PMC4768623
- Fishbain DA, Cutler R, Rosomoff HL, Rosomoff RS. Chronic pain-associated depression: Antecedent or consequence of chronic pain? A review. The Clinical Journal of Pain. 1997;13(2):116–137
- Babel A, Taneja R, Mondello Malvestiti F, Monaco A, Donde S. Artificial Intelligence Solutions to Increase Medication Adherence in Patients With Non-communicable Diseases. Front Digit Health. 2021 Jun 29;3:669869. doi: 10.3389/fdgth.2021.669869. PMID: 34713142; PMCID: PMC8521858

